By Heidi Singer
University of Toronto researchers are addressing hospital crowding in the most counter-intuitive way imaginable – by seeking out patients far beyond their hospital’s overburdened corridors.
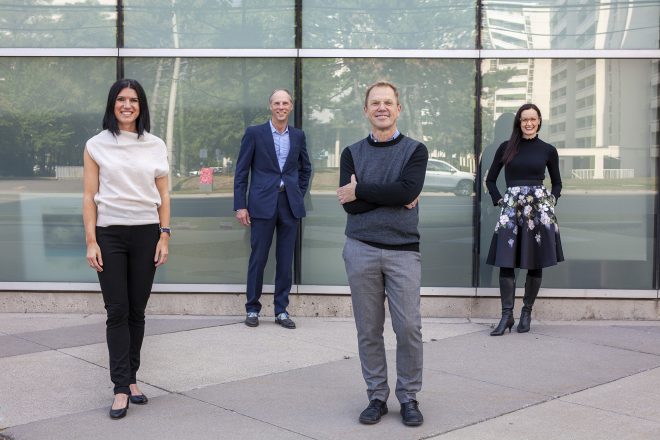
Prof. Laura Rosella uses data and analytics to identify populations at risk of chronic conditions. Prof. Kerry Kuluski talks to patients and families, adding crucial context to the data. And Prof. Walter Wodchis turns this information into action.
These faculty members at the Institute of Health Policy, Management and Evaluation, which is within the Dalla Lana School of Public Health, are part of an increasing wave of public health and health systems researchers who believe that in order to translate their findings into real, timely change, they must have an intimate understanding of – and relationship with — the institutions and communities they wish to influence. And in one large Mississauga hospital system, they believe they’ve found the perfect partner.
“For me, research is not about discovery for its own sake – it’s about having impact,” says DLSPH Prof. Rob Reid, the Canadian-born, American-trained physician scientist leading the charge. “Health systems across the world are broken, with too many people left behind, and I believe research can have a strong role to play in changing how they bring value to the populations they serve. We’re combining high-powered research methods with expertise in rapid implementation – it’s quality improvement on steroids.”
DLSPH researchers are now deeply involved in the three campuses that make up Trillium Health Partners (THP), the sole hospital system serving about 1 million residents of Mississauga a diverse and rapidly growing city, and many more in the surrounding area. They are analyzing data, and creating indicators and dashboards with multiple data sources from the hospital and the community. They are talking to people with complex medical needs, diabetes and mental health challenges. They are sitting with patients and their families to understand what good care means to them. And most importantly, they have a plan for how that information will be used to improve care and planning immediately and tangibly – not theoretically, and in some distant future.
In short, they are helping to turn a community hospital system into Canada’s first learning health system.
The system they are creating is one that can constantly shift, reacting to new information, generating data and learning from it; creating change, analyzing the results, assuring that care reaches everyone, then readjusting, and then doing it all again. That’s how a learning health system is described in academic papers, hashtags and case studies. But, says Reid, nowhere in the world is it truly and consistently happening at scale.
It can be hard to explain the revolutionary nature of a learning health system to those who, understandably, assume it already exists. Afterall, Canada is thought to have a health system meant to serve everyone, instead of a collection of insurance programs. And surely someone must be learning from all the questions patients are constantly being asked.
But most of that information doesn’t travel far. It may be used to improve services in one particular area, but rarely does anyone study whether the right questions were asked or whether the improvement made a difference. Health systems are not set up to learn from themselves – certainly not in the short term, Reid says. And all of this is much tougher when you want to reach people facing barriers to care, who are invisible to the hospital until they come in through the emergency department.
The transformation now happening in Mississauga could show the way. One hospital system, many community organizations and residents are learning to work together to improve health. They are using technologies both high and low to understand and refine their knowledge of what people need to keep themselves healthy and out of the hospital. And they are racing against a demographic clock.
Why Mississauga, Why Now?
The need to reach out to people where they live comes from an impending population boom in Mississauga. With only one hospital system, and an increasingly diverse, fast-growing population, hospital leaders know they can’t meet future needs by doing things the same way. And they can’t build their way out of the crisis: Even with current expansion plans, hospital capacity will remain over-stretched.
“There is absolutely a fundamental capacity problem that is becoming more urgent by the year,” says Reid. “Many institutions would simply hunker down and focus inward when faced with a challenge like this. Rather I saw a hospital that wants to change how it fundamentally operates – and a city with a real can-do attitude. I saw a huge opportunity.”
Reid became a convert to this idea that health systems can learn from themselves two decades ago. In the late 90s, he was a young Canadian physician with a PhD in health policy, working in B.C. and writing research reports that sat on shelves. He heard about a Health Maintenance Organization (HMO) in Seattle called Group Health Cooperative that was proactively trying to keep its million customers healthy and satisfied.
This non-profit, integrated healthcare system had a research institute that was more like a company’s R&D operation. They used it to invent new ways to make things better, cheaper, and faster. In collaboration with system leaders, its researchers spun out a model to improve the health of patients with diabetes and other chronic diseases, and then its clinicians tested it, finding it led to substantial improvements. The Chronic Care Model spread around the globe, including in Canada, and was eventually adopted by the World Health Organization.
At Group Health, Reid was able to design, implement, and test one of the world’s first patient-centred systems, where each person had a medical ‘home.’ That work on primary care redesign, was used across the US and in other parts of the world to assist with reforming primary care. It led to a seminal 2012 paper, published by Reid and colleagues, about how a learning health system should operate.
But problems with the American system of healthcare payment felt overwhelming and intractable, and Reid didn’t see himself staying forever. In 2015, he began looking for a Canadian institution interested in working with him to apply what he had learned in Seattle. At the time, THP had just formed and struck a partnership with the University of Toronto which allowed the hospital system to reinvent its research institute.
“I found Mississauga and they found me because we had a desire to do the same thing,” he says. “The Board wanted an embedded research unit that was system-oriented and could help solve their huge capacity problems – novel thinking in Canada. The mission of the hospital was to develop a new kind of health care for a healthier community – not just hospital patients but an entire community.”
The hospital system wanted to use the advances already discovered and learn how to apply them to patients at the right time and place and in the right way, making sure everyone could get through the doors when they needed to. “Instead of focussing on traditional clinical research, they wanted to focus on systems, services and population health,” says Reid. “And that’s why a public health school was the natural partner.
Around the same time, the currents were shifting at the Dalla Lana School of Public Health, itself a newly formed faculty with its first ever academic plan, published in 2019, that focussed on creating impact from research. Dean Adalsteinn (Steini) Brown, a former Ontario Assistant Deputy Minister of Health, was particularly focussed on striking research partnerships that would allow faculty to help foster truly sustainable and higher-performing health systems. He, along with IHPME faculty members, were already very interested in learning health systems, and several years ago began to embed postdoctoral researchers into Ontario Health Teams.
Championing Change
Reid came to THP as the first Chief Scientist and Hazel McCallion Research Chair in Learning Health Systems at the hospital’s newly formed Institute for Better Health. He began teaching at DLSPH, where he met Rosella, Wodchis and Kuluski. Each was a seasoned researcher who brought something very different, but complimentary, to the table. And each wanted their research to have a tangible impact.
Prof. Laura Rosella is an epidemiologist and leading expert in Big Data and Population Health Analytics with a focus on the prevention of chronic diseases like type 2 diabetes. She analyzes huge amounts of data using a range of novel analytic approaches, and helps to understand segments of the population with unmet needs; all with an equity lens.
Rosella joined the Institute for Better Health as the Stephen Family Research Chair in Community Health just before COVID touched down in Canada. She had been intrigued by Reid’s vision that researchers could make a real difference in population health at THP.
Today, Rosella’s analysis allow hospital leaders to understand how best to deploy resources to tackle health problems in the community – reaching people before they come through the door.
“I’m interested in people’s health information but also the broader socioeconomic and wellbeing factors that determine health outcomes,” she says. “And that includes all aspects of community wellbeing. We analyze environmental, health and social data to understand who is at risk for certain outcomes in the community and who should be our priority.”
Rosella and THP leaders compiled the first health data report on the population served by the hospital, which highlighted how various social, environmental, and economic factors varied across the population and determined hospital use. Over the COVID-19 pandemic, Rosella brought these data together to inform hospital capacity planning and broader testing and vaccination strategies to improve the wide disparities seen in the region. More recently, she is examining who is at risk for preventable conditions and dying prematurely from them.
“We can identify groups in the population that are at high risk of dying prematurely, and now we’re working with the local Ontario Health Team, Mississauga Health, to integrate those insights into planning for targeted proactive and preventive health services in the community,” Rosella says.
But the data only tell part of the story. Rosella works with fellow DLSPH Prof. Kerry Kuluski to put their findings in front of people — actual patients, their caregivers and families — to ask what’s missing. Patients add the crucial context: for example, the average 45-year old in Mississauga might be caring for elderly parents, working two jobs among many challenges and demands, all of which affects their health.
“Before, this information might come from looking at admission data or patient surveys, but now it’s both plus much more comprehensive quantitative and qualitative data,” says Rosella. “That’s where the innovation is happening.”
Bringing these streams together is possible because of Kuluski’s many years of working with patients and their families to better understand their needs and improve their experiences. In Canada, health systems are largely designed for providers, she says. But patient input is only as good as the researcher’s access to them. And traditionally it has been tough for non-clinicians to spend enough time with patients to build those relationships.
“We’ve been working on how to improve the way we collect patient experience data, by doing things like creating a shorter version of the surveys we use that has more actionable information as well as learning from our surrounding communities how they wish to engage and share information about their needs,” says Kuluski, who teaches patient and caregiver research and engagement at IHPME. “We are learning how to collate different types of experience data, including survey results, feed it back to the teams and then work together to amplify what’s working well and change what’s not.”
Two of her PhD students, Umair Majid and Emily Cordeaux, are working on dissertations at THP, and their findings will be used by the hospital system to to partner with patients and families from the bedside all the way to decision making tables.
“We’re deliberately putting research and practice together in ways we haven’t really done before,” says Kuluski. “In health systems research, the the old model is to work in silos and focus on writing manscripts. Now there is a shift to work and learn with patients and communities to make a more meaningful impact. We’re breaking out of our silos to bring the worlds of research and practice together to make the health care system work better.”
And finally, THP needs to understand how to implement the plans developed by data and patient surveys. A fellow DLSPH researcher, Prof. Walter Wodchis, is an expert in rapid evaluation and implementation.
“We bring the capacity to look across the whole system and now to collaborate across care,” says Wodchis, who, along with Kuluski, is based at IHPME. “Hospitals don’t know how to choose indicators and look at quality on the system level. That’s what DLSPH brings. And it’s really important for people with complex health needs.”
Few people want to spend their last days in hospital, but in Mississauga, an unusually large proportion do. Wodchis found that few people outside hospitals at high risk of dying within six months received palliative care. Now the DLSPH team is using approaches designed to learn quickly whether their changes improve the end-of-life experience and whether more would help.
“The way we’re working with the palliative team is the way we want to work everywhere: collect the data, co-design a solution, rigorously evaluate it with an open mind, asking ‘how can we just get better?’” says Wodchis. “We’re doing exactly what should happen because we finally found a place where what should happen can happen.”
For the DLSPH team, evidence-informed change is the point, but change is generally also the problem. Health care, being a high stakes profession, is slow to transform. The doctor’s credo “first do no harm” can create risk adversity, since it’s much safer to be blamed for missed opportunities than for failure.
But these champions of change are confident that it is happening in Mississauga. First, the hospital CEO is strongly behind it, and hundreds of staff are specifically trained in change management.
“We’re redefining the role of the hospital in the Canadian context,” says Karli Farrow, THP’s president and CEO. “This is no longer only about high quality acute-care services delivered to those who make their way to us. Our goal is better health for the community, which means we need to be a part of a complete and inclusive system of care. Our research mission is completely embedded into this effort.”
And the team had an accelerated experience with COVID, where Mississauga was hit hard but had a strong response anchored in data and modelling. Rosella worked with hospital leaders and was able leverage local data to predict surges and target prevention to specific populations and areas.
In the hospital’s clinical programs, fear of scrutiny is addressed head on, and now people are asking Wodchis to evaluate their own programs. Rather than being seen as a test of their value, teams are viewing evaluation as vehicle to rapidly improve and meet the patients and community needs in a better way.
Turning a handful of programs into a learning health system will take time, Wodchis acknowledges. “I think once we have 50 under our belt and we’ve got 20 running each year, we’ve got a health system in place, because then we’ve got scale,” he says. “It’s not going to happen quickly or easily, but being able to do this for a million people is something I’m pretty confident in.”
And ultimately, the DLSPH research team is most interested in showing that learning health systems can be applied anywhere. “At the end of the day, this work still has to be done locally because these changes are built on relationships and trust,” says Wodchis. “But the approach is entirely scalable.”
Much like the models of care he helped developed in the 90s, Reid, too, would like to see the THP example copied around the world. The ambition is huge, but so is the potential payoff. “We’re taking a large, complex community hospital system and building a health system where we anticipate needs and reach out to surprise and delight patients with proactive care,” he says. “Patients might not feel the difference yet because we’ve just started – but they will.”
Related News

Sign up for IHPME Connect.
Keep up to date with IHPME’s News & Research, Events & Program, Recognition, e-newsletter.
Subscribe to Connect Newsletter
Get in Contact
Communications
Marielle Boutin
Email Address: ihpme.communications@utoronto.ca





